This topic takes on average 55 minutes to read.
There are a number of interactive features in this resource:
 Human biology
Human biology
 Biology
Biology
 PSHE / Citizenship studies
PSHE / Citizenship studies
Insulin is a 51 amino acid protein and needs to be injected into the body rather than taken orally to avoid being broken down in the digestive system.
Early insulin treatments used the hormone isolated from cow (bovine) and pig (porcine) pancreas. This needed a great deal of purification to isolate the insulin and even then, there were contaminants. The preparations were short-acting and could cause allergic reactions.
In 1955, the amino acid sequence of human insulin was discovered. The amino acid sequence of porcine insulin is different to human insulin by one amino acid. Bovine insulin differs by three amino acids.
Modern insulin is now obtained from bacteria that have been genetically modified to produce human insulin. By further manipulating the insulin, it has been possible to develop a range of medications that have different properties. For example, adding zinc causes the insulin molecules to form hexamers (six insulin molecules loosely attached to each other). This form of insulin is absorbed into the body more slowly than regular insulin, thus reducing the need for more frequent insulin injections.
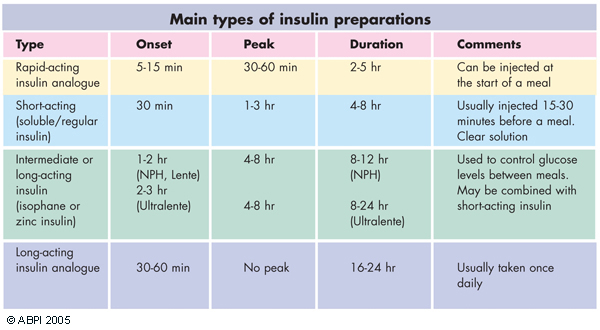
Range of insulin preparations, from short acting to long acting.
Injecting insulin on a regular basis can cause problems and researchers are constantly working to develop better ways to take insulin.
Skin patches are being developed that allow the insulin to be directly absorbed into the body and implants under the skin may also be a treatment of the future.
Small pumps which inject insulin under the skin in a controlled way throughout the day are now available. Miniaturised 'nanopumps' may soon replace the large pump shown here.
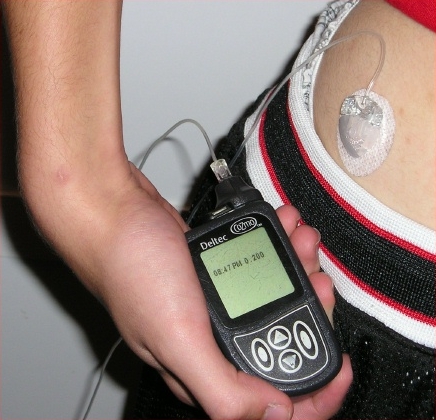
Pumps deliver controlled amounts throughout the day.
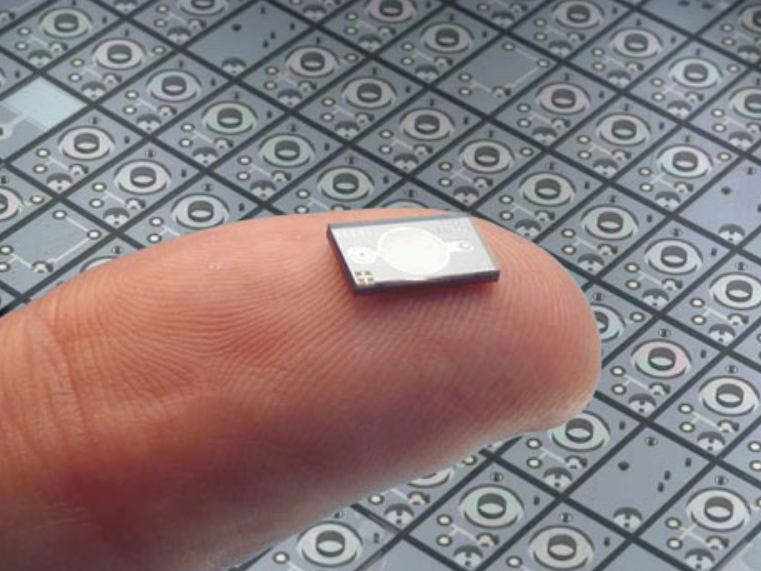
Using nanopumps may allow insulin to be delivered from pumps the size of skin patches. Courtesy of: Insulin Nanopump™ from Debiotech SA, Switzerland
Inhaled insulin-powders have been developed to enable the hormone to be absorbed directly into the blood from the nose and mouth mucosa. This bypasses the digestive system. These have so far proved unpopular with patients and their use is limited.
Transplants of the pancreas and islet cells from donors are becoming more common treatments. People with diabetes, particularly if they have associated kidney disease that requires a kidney transplant, may be given a whole pancreas from a donor. More commonly people with diabetes may be given donor islet cells. These donor cells are isolated from the several donors and then injected into the hepatic vein. From here they travel in the blood and become lodged within the liver and produce insulin. This procedure is called islet cell embolisation. As a result of both of these procedures insulin production in individuals with type 1 diabetes is reinstated and they no longer have to inject insulin.
In the future it may be possible to grow large numbers of beta cells from stem cells in the laboratory. This would be a much more readily available supply of insulin-producing beta cells which can then be used for islet cell embolisation.
Lifestyle changes play a key role in the management of type 2 diabetes, and initial steps include regular physical activity, a balanced diet and loss of any excess weight. For a large proportion of people with type 2 diabetes, changes to their lifestyle will reduce their blood glucose levels sufficiently. However if levels remain high even with these changes, then medication is usually required.
There are five types of medicines that are used to treat type 2 diabetes. However, these should be used in addition to a change in lifestyle. The groups of medicines are:
Long-acting insulin may, if necessary, be administered once a day.
Use the statements below and the information on this page to produce a table that summarises the similarities and differences between the treatments for Type 1 and Type 2 diabetes.
