This topic takes on average 55 minutes to read.
There are a number of interactive features in this resource:
 Biology
Biology
Stem cell research is an exciting new area in biotechnology. Although it has not yet produced a mainstream cure for people, there are some very effective treatments in place for horses, and human trials are progressing fast. This research is still very young: embryonic stem cells were only first cultured in 1998, and iPSCs first created in 2006. Therefore, the clinical trials using stem cells already underway are mainly testing their safety rather than their capabilities. Fortunately, stem cells don’t need to be transplanted into someone to act as a treatment: research in the lab using stem cells as disease models offers a way of testing new drugs and carries fewer risks than human stem cell trials.
Experimental evidence that stem cell therapy does work continues to grow. Here you are going to look at progress using stem cell therapies in a number of different areas of human health, starting with the cardiovascular system.
Cardiac progenitor cells are tissue stem cells found in the heart which can differentiate to form cardiomyocytes. During a heart attack, areas of heart muscle are damaged and can’t repair themselves, which may lead to heart failure.
Unfortunately, the body’s ability to produce new cardiomyocytes decreases with age, as the likelihood of a heart attack increases – and so the mammalian heart shows little potential to regenerate without medical help. It is already known that zebrafish can repair damage to their hearts following a heart attack – it is thought that by introducing stem cells into the damaged area or stimulating local cardiac progenitor cells mammals could also be able to repair heart damage.

This is not something that is routinely performed on humans, but trials in other mammals have shown promising results: mouse stem cells can repair damaged areas of mouse hearts when introduced after a heart attack, whilst human stem cells show the same effect when introduced into damaged rat hearts following a heart attack. Trials are currently underway to investigate whether adult stem cells can help hearts recover from both heart failure and from heart attacks. Some very positive results are emerging. For example, in one small scale study published in 2016 in the Journal of Cardiovascular Translational Research, 11 patients having bypass surgery also had stem cells injected into their heart muscle where there was scar tissue from previous heart attacks. All of the patients were at very high risk of dying at the time of the procedure, but 24 months later they were all still alive and there was a 40% reduction in scarring, a 30% improvement in heart function and a 70% improvement in quality of life. Of course the patients had heart bypass surgery which would improve their condition too, but the reduction of scar tissue and increase in function excited scientists. A large-scale controlled study of this technique was done in London in 2017.
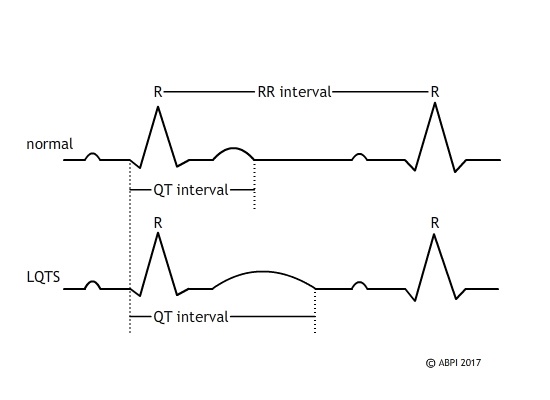
Although one of the major goals of stem cell technology for the future is to develop therapies which can be used to repair damage caused by a disease or injury, it already plays a major role in investigating diseases. Animal models have a limited value because there are differences between the hearts of all species of mammals. For example, long QT syndrome is a rare genetic disease that can lead to the sudden death of young people. It takes the heart muscle longer to recover after each beat, and it can result in arrhythmias which can be fatal.
iPSC and ESC technology offer scientists the opportunity to model the disease: iPSCs and ESCs from patients suffering from long QT syndrome have been differentiated to form cardiomyocytes which contain the mutant DNA that causes the disease. There are a number of different mutations which all result in similar disease, but which respond differently to potential treatments. Stem cells derived from affected patients have been grown, differentiated to give cardiomyocytes and then used in conjunction with normal cardiomyocytes to study the mechanisms of the disease at the molecular level, to identify mutations for potential gene therapy and to test possible treatments.